Living With and Managing Glaucoma
How do I live with and manage my glaucoma?
Living with and managing glaucoma can seem daunting to a newly diagnosed glaucoma patient, however, by taking some practical steps and working closely with an experienced ophthalmologist, glaucoma patients can continue to enjoy active lifestyles and maintain good ocular health. The fellowship-trained ophthalmologists at Glaucoma Associates of Texas encourage patients to be organized and well-informed, while making healthy choices, communicating with their doctors, and carefully complying with their glaucoma treatment plans.
Living With and Managing Glaucoma
How do I live with and manage my glaucoma?
Living with and managing glaucoma can seem daunting to a newly diagnosed glaucoma patient, however, by taking some practical steps and working closely with an experienced ophthalmologist, glaucoma patients can continue to enjoy active lifestyles and maintain good ocular health. The fellowship-trained ophthalmologists at Glaucoma Associates of Texas encourage patients to be organized and well-informed, while making healthy choices, communicating with their doctors, and carefully complying with their glaucoma treatment plans.
Living With and Managing Glaucoma
How do I live with and manage my glaucoma?
Living with and managing glaucoma can seem daunting to a newly diagnosed glaucoma patient, however, by taking some practical steps and working closely with an experienced ophthalmologist, glaucoma patients can continue to enjoy active lifestyles and maintain good ocular health. The fellowship-trained ophthalmologists at Glaucoma Associates of Texas encourage patients to be organized and well-informed, while making healthy choices, communicating with their doctors, and carefully complying with their glaucoma treatment plans.

Stay Organized
Glaucoma patients often need to take several medications and/or administer medicine several times per day. Establishing a routine for taking glaucoma medications will help avoid missing doses or accidentally taking medicine twice. Taking medications around specific times, such as upon waking, at mealtimes, and before bedtime, can keep glaucoma patients on a set schedule.
If you tend not to have routine mealtimes, consider setting a phone or watch alarm as a reminder. If a dosage is missed, take the medicine as soon as possible and return to your regular glaucoma treatment schedule.
Additional glaucoma medication tips include:
- Keep a log of the type and frequency of medications you take, and carry this record in your wallet or purse.
- Be sure to refill glaucoma prescriptions in a timely manner as not to run out.
- If possible, obtain and fill a back-up prescription in case your medication is lost or you need to travel on short notice.
Managing and organizing your schedule can also be important for glaucoma patients, especially if driving is difficult. Night vision can become problematic with glaucoma, so trips and outings may need to be planned around daylight hours. For evening events, scheduling a ride may be necessary.
Other organizing suggestions for glaucoma patients include:
- Schedule future eye check-ups before leaving each ophthalmologist appointment, and place it on your calendar as soon as possible.
- Bring a friend or family member with you to eye appointments. Having “extra ears” can be helpful for remembering doctor instructions on medication, as well as nutrition and lifestyle changes that may need to be made (especially for newly diagnosed glaucoma patients).
- Make a habit of writing things down, such as:
- Questions you want to ask your doctor
- Changes in your condition
- Medication problems
- Doctor instructions
Be Informed and Communicate About Your Glaucoma
Knowing as much as you can about your glaucoma will help you manage it more successfully and decreases your risk of experiencing problems, such as misunderstanding doctor instructions or improperly dispensing medication. Being an informed glaucoma patient will also help you utilize support groups, occupational therapy, and assistive devices to make living with glaucoma easier.
Know what medications you take and how often, especially when visiting other healthcare professionals. Be sure to tell any other doctors you see that you have been diagnosed with glaucoma so that they can coordinate medication if necessary.
Family members should be aware that you have glaucoma as they will be at greater risk for developing glaucoma. Since glaucoma typically has no symptoms at its onset, early detection is key to successful treatment, and relatives should have regular eye exams as a precaution.
Talk to Your Glaucoma Doctor
Let your ophthalmologist know if you have any side effects with your glaucoma medication or have any changes in your routine. Ask questions about anything you are unsure of or need help with. Be sure you know how to use your eye drops properly for best results in treating your glaucoma.
Report any changes in vision or eye problems, such as:
- Eye irritation
- Watery eyes
- Blurriness
- Eye discharge
- Cloudy vision
- Halos or rainbows around lights
Having an open line of communication with your glaucoma specialist is imperative. Be honest about your compliance with glaucoma treatment so your doctor can effectively treat your condition. At Glaucoma Associates of Texas, we are always willing to discuss any aspect of your glaucoma and are committed to helping you successfully manage it by preserving vision and offering support through education and quality care.
Eye Drops & Healthy Choices for Glaucoma
How to Use Eye Drops
Glaucoma eye drops to lower intraocular pressure are the most important form of initial treatment for glaucoma. Despite their widespread use, many patients do not know how to apply them correctly. Fortunately, there are several ways to do this effectively. Using a mirror or having someone else give you the eye drops may make this procedure easier.
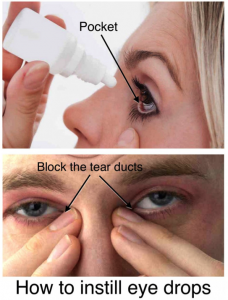
Instilling Glaucoma Eye Drops
- Wash your hands thoroughly with soap and water.
- Use a mirror or have someone else put the drops in your eye.
- Remove the protective cap. Make sure that the end of the dropper is not chipped or cracked.
- Avoid touching the dropper tip against your eye or anything else.
- Hold the dropper tip down at all times to prevent drops from flowing back into the bottle and contaminating the remaining contents.
- Lie down or tilt your head back.
- Holding the bottle between your thumb and index finger, place the dropper tip as near as possible to your eyelid without touching it.
- Brace the remaining fingers of that hand against your cheek or nose.
- With the index finger of your other hand, pull the lower lid of the eye down to form a pocket. (Fig. 1)
- Drop a single eye drop into the pocket made by the lower lid and the eye. Placing drops on the surface of the eyeball can cause stinging. Using more than one eye drop will cause overflow and waste.
- After applying the drop, the eyelids should be gently closed for about two minutes to allow time for the medication to be absorbed into the eye.
- Although you may feel like blinking, you should try to avoid this. Blinking may squeeze the drop out of the eye and into the tear duct which leads into the nose. By gently closing the lids, the medication will remain in contact with the eye so that it can be absorbed.
- Block the tear ducts with your thumb or index finger for two minutes as the eyelids are gently closed, so the flow of the drop and the tears into the nose can be avoided (Fig. 2).
- Replace and tighten the cap right away. Do not wipe or rinse it off.
- Wipe off any excess liquid from your cheek with a clean tissue. Wash your hands again.
Using More Than One Eye Drop
If you are using more than one eye drop, you should wait at least 5 minutes before applying the second eye drop to have it absorbed best. The lower lid pocket into which the drop is placed is small and can hold a little more than one drop at a time. Placing more than one drop at a time causes an overflow, and washes the eye drop from the eye.
Bring your eye drops with you every time you have an appointment with your eye doctor. Your eye doctor can help you learn to use your eye drops correctly.
Healthy Choices for Glaucoma
Managing glaucoma involves making healthy nutrition and lifestyle choices that will enhance ocular health.
Glaucoma eye-care tips include:
- Follow your ophthalmologist’s instructions closely. Compliance with glaucoma treatment is the most important step you can take in preserving your eyesight.
- Keep your eyes clean and irritant-free.
- For women, use non-allergenic eye make-up, and replace it frequently.
- Avoid rubbing the eyes if they feel itchy (some glaucoma medicines can cause temporary blurriness or scratchy eyes).
- Utilize goggles during swimming and protective eyewear during sports or yard work.
- Eat foods that promote healthy eyes, such as leafy green vegetables and other foods high in antioxidants.
Other Health Tips for Successfully Managing Glaucoma Include:
- Get enough exercise. Studies show that regular exercise can reduce risk factors for glaucoma and help maintain intraocular pressure (IOP). Check with your ophthalmologist before beginning any exercise program.
- Minimize salt and caffeine use to keep blood pressure in check.
- Do not smoke.
- Reduce stress by making time to relax and take part in activities you enjoy.
Living with glaucoma usually involves some change in lifestyle, however, following your treatment plan, being informed and organized, communicating with your doctor, and maintaining good general health will help you successfully manage glaucoma. If you have been diagnosed with glaucoma or are at high-risk for glaucoma and would like more information about preserving your vision, contact the Glaucoma Associates of Texas for an appointment.
Contact Our Office to
Learn More
Learn More